
How come health officials and the media are not honestly exploring why?
The first confirmed COVID-19 case in Africa was on February 14, 2020 in Egypt. The first in sub-Saharan Africa appeared in Nigeria soon after. Health officials were united in a near-panic about how the novel coronavirus would roll through the world’s second most populous continent.
By mid-month, the World Health Organization listed four sub-Saharan countries on a ‘top 13’ global danger list because of direct air links to China. Writing for Lancet, two scientists with the Africa Center for Disease Control outlined a catastrophe in the making:
With neither treatment nor vaccines, and without pre-existing immunity, the effect [of COVID-19] might be devastating because of the multiple health challenges the continent already faces: rapid population growth and increased movement of people; existing endemic diseases…; remerging and emerging infectious pathogens …, and others; and increasing incidence of non-communicable diseases.
Many medical professionals predicted that Africa could spin into a death spiral. “My advice to Africa is to prepare for the worst, and we must do everything we can to cut the root problem,” said Tedros Adhanom Ghebreyesus, the first African director-general of the WHO warned in March. “I think Africa, my continent, must wake up.”
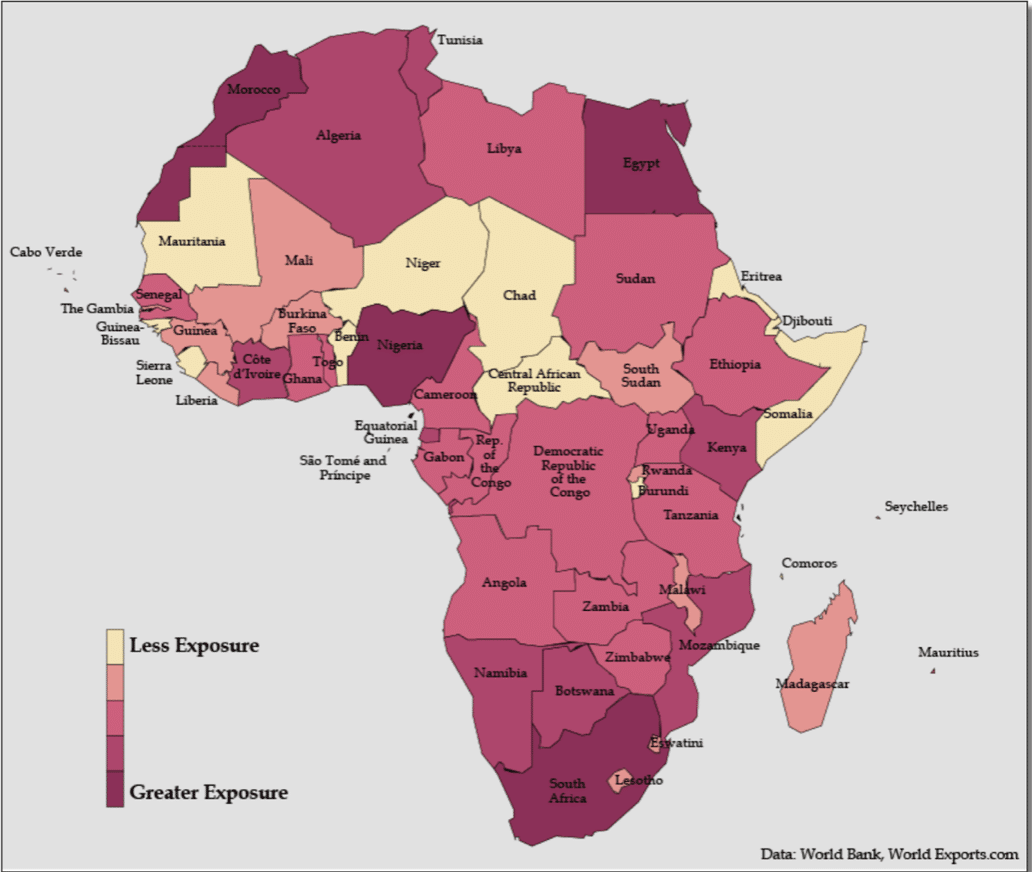
By spring, WHO was projecting 44 million or more cases for Africa and the World Bank issued a map of the continent colored in blood red, anticipating that the worst was imminent.
Dire warnings seemed to make sense. After all, the vast majority of the world’s poorest people reside in the region, struggling with unhygienic environments, conflict, fragmented healthcare and education systems and dysfunctional leadership — all factors that could light a match to the tinder of the SARS-CoV2 outbreak. Scientists say that most African countries lack the capacity and expertise to manage endemic deadly diseases like malaria?
Each individual’s risk of dying of a particular disease tends to reflect access to adequate health care and underlying health conditions (co-morbidities). Those factors have proved to be a toxic mix in poorer communities in the United States, Brazil, UK and other countries where lower income groups, often ethnic and racial minorities, are dying at rates higher than others. Africa seemed ripe for catastrophe.
But disaster never came. Africa has not been affected on anything near the scale of most countries in Asia, Europe, and North and South America. (The major exceptions being China, Taiwan, Australia and New Zealand, which zealously enforced lockdowns). In fact, the vast African continent south of the Sahara desert, more than 1.1 billion people, has emerged as the world’s COVID-19 ‘cold spot’.

Note: ‘Africa’ includes the mostly White countries of North Africa, which have been far harder by COVID than sub-Saharan Africa]
The latest statistics show about 3.8 million cases and 100,000 coronavirus-related deaths, concentrated mostly in the Arab majority countries north of the Sahara. Except for South Africa, the most multi-ethnic of the Black majority countries, and Nigeria, sub-Saharan Africa has largely been spared.

Courtesy: Africa CDC
According to Worldometers, by late-February, Europe, with less than 2/3 the population of Africa, had almost 33,000,000+ cases, 900% more, and almost 800,000 deaths, 800% more. The US, with less than 1/3 the number of people, has 2900% more cases and 2400% more deaths, according to stats compiled on Wikipedia.

Journalists and even some scientists have been twisting themselves into speculative pretzels (here, here, here) trying to explain this phenomenon. Theories range from sub-Saharan Africa’s ‘quick response’ (no); favourable climate (which did not protect Brazil and other warmer climes in South America); and good community health systems (directly contradicted by WHO and Africa CDC).
In each of those articles acknowledging the “puzzling” statistics, journalists were sure to suggest Armageddon might be right around the corner. “Experts fear a more devastating second surge,” warned National Geographic in late December, although there was no first surge and just two weeks before Africa’s tiny December uptick (driven almost entirely by the mutant variant in South Africa) turned back downward, according to Reuters.

Why Africa has been less impacted by COVID-19
What’s going on here? And why are the media and most scientists so unwilling to engage the most likely scenario: Black Africans appear to be protected in part by their ancestral genetics. Combined with the fact that sub-Saharan Africa is the youngest region in the world—youth brings fewer co-morbidities and age is the most significant factor in contracting and dying from COVID-19—DNA is the most likely explanation for sub-Saharan Africa’s comparatively modest case and death count.
Except for one research project in Hawai’i, scientists have all but ignored exploring the population genetics angle, almost certainly fearful of stirring the embers of race science.
“It is really mind boggling why Africa is doing so well, while in US and UK, the people of African ancestry are doing so poorly,” Maarit Tiirikainen, a cancer and bioinformatics researcher at the University of Hawai’i Cancer Center, told us in an email.
Dr. Tiirikainen is a lead researcher in a joint project at the University of Hawaii and LifeDNA in what some believe is a controversial undertaking considering the taboos on ‘race’ research. They are attempting to identify “those that are most vulnerable to the current and future SARS attacks and COVID based on their genetics”.

Maarit Tiirkainen
Blacks (along with other ethnic minorities) in the US and Great Britain have generally fared worse than Whites in contracting COVID-19 and surviving it. “For the latter, it seems the western socioeconomics may play a major role. There may also be genetic differences in immune and other important genes,” Dr Tiirkainen wrote.
(Note: The terms ‘Black’ and ‘White’ are used as shorthand for more cumbersome expressions like ‘those of African descent’ or ‘people of European ancestry’. As addressed below, ‘Black’ and ‘White’ are not science-based population categories.)
Dr. Tirikainen, like many researchers in this field, when communicating candidly, is skeptical that social and environmental factors alone can account for the extraordinarily low COVID-19 African infection and death rates. It is not because Africa took extraordinary steps to insulate itself as the pandemic spread. Health care remains fragmented at best. COVID information outreach has been limited by scant resources.
At the end of March, when much was still to be learned about the science of COVID-19, co-authors of this article — Genetic Literacy Project’s Jon Entine and contributing science journalist Patrick Whittle — discussed some of the potential reasons in the article What’s ‘race’ got to do with it?.
After discussions with many experts, we decided not to reflexively exclude genetic explanations, which are always a taboo subject. Rather, we examined the panoply of likely causes, rejecting the a priori Western prejudice that often excludes evidence that might be linked to population-level genetics and group differences for fear of ‘racializing’ the analysis. Note we are very aware that skin color is not a recognized science-based population concept. Given the racist history of biological beliefs about human differences, addressing the fact of ancestrally-based genetic differences must be pursued carefully.
Why even discuss possible genetic factors? Because biases among researchers and public policy officials could undermine the development and deployment of treatments and antiviral vaccines for all of us, but particularly for more vulnerable populations in Africa, and in the African diaspora. Identifying those with genetic resistance to infection or who may be genetically protected in some degree from developing symptoms could help scientists develop treatments for all of. Lives are at stake.
So let’s dip our toes back into these murky waters. Could our ancestry, which defines our genetic make-up, play a role in disease susceptibility, for COVID or other viruses?
Environmental-based Black-White differences impact COVID vulnerability
There are some significant non-genetic factors behind the Africa numbers. In the case of disease susceptibility, social and environmental explanations have played a huge role in the limited impact so far of COVID-19 in Africa. For one, the apparent low incidence of cases and deaths could be due in part to under-reporting or limited testing, although testing has been surging in Africa even as the number of cases remained flat.
The most significant environmental factor, scientists say, is age. The average age of Europeans is 43; it’s 38 in the US; across the African continent, it is 18. The average age in Niger, Mali, Uganda and Angola is under 16. While roughly a quarter of the population in both Europe and North America is over 60-years old, in Africa, the 60+ age cohort makes up only 6 percent of the population.

The young, when infected, are also less apt to show symptoms. Asymptomatic people are not as likely to be tested, perhaps suppressing the numbers. Younger people are, by and large, healthier. The average age of Black Americans is about twice as old as Black Africans. Moreover, the deaths among African Americans — almost twice that of White and Asian Americans — has been almost exclusively concentrated among the elderly, many with multiple co-morbidities and less access to health care. That’s the opposite of the situation in Africa.
The younger African population may explain some of the disparities in deaths, but not all of them; the wealthier nations of Asia have managed the pandemic better than Europe and North America, despite having similarly older populations, and the virus is raging in some South Asian countries.
It also should be noted that age has often played the opposite role in surviving scourges. Malaria is historically the world’s deadliest disease. But age-related survival rates are the reverse of that with COVID-19, with the very young most at risk. In 2018, for example, most of the estimated 405,000 people who died from malaria were young children in sub-Saharan Africa.
Climate also may play a role. Generally, the pandemic has spread more virulently in colder climes, with more temperature countries in Asia and Africa somewhat spared from the scourge. But most of those countries, from Australia, across China to Taiwan, have undertaken massive tracing and have imposed near universal shutdowns on occasion. African countries have been less proactive, constrained in large part by a lack of funds.
Genetics and COVID
To what degree does ancestry play in role in our susceptibility to COVID-19?
Unfortunately there is a dearth of research on the genetics of African peoples, so it’s difficult to make too much of these fragmented examples. And despite Africa being the “cradle of humankind”, and with its populations containing more human genetic variation any other continent, Black Africans and those of African descent remain woefully underrepresented in genetic studies.
Given the historical research bias towards Eurasia and North America, almost 20 years after the sequencing of the human genome, the vast majority of genetic samples are of European ancestry (nearly 90 percent in 2017, with most of these from just three countries — Great Britain, US and Iceland). Recent pioneering surveys of African genomes are just now beginning to reveal the continents’ rich genetic legacy, replete with the merging and divergence of myriad ancestral populations.
What genetic factors could be in play impacting COVID-19 infection and death rates? Research and informed speculation is already underway.
An earlier study on the possible contribution of genetics to the SARS-CoV2 infection found significant population-based differences in ACE2 receptors that modulate blood pressure in the cells located in the lungs, arteries, heart, kidneys and intestines. Africans are considerably less likely than East Asians to express the ACE2 receptors, though slightly higher than Europeans, the researchers believe.
“There have been major differences in the rates of SARS-CoV-2 infection and the severe disease between the different geographic regions since the beginning of the COVID-19 pandemic, even among young individuals,” wrote Dr. Tiirikainen. “There may also be genetic differences in immune and other important genes explaining why some people get more sick than others.
At least two studies show that blood type O could be associated with a lower risk of COVID-19 infection and reduced likelihood of severe outcomes, including organ complications. There is also some evidence that those with blood type A are more susceptible to COVID-19. The researchers did not find any significant difference in rates of infection between A, B and AB types. About 37 percent of the world population is O+ and 6 percent is O-. About 50 percent of Africans have blood group O, the highest in the world.

It’s well established that certain HLA (human leukocyte antigens) alleles confer susceptibility to specific diseases. African-descended and European-descended populations implicate distinctively different immunity responses in dozens of diseases treatments. For example, it is extremely rare for people of unmixed Black African ancestry to get ankylosing spondylitis, a rare type of arthritis. Whites are three times more likely to get it. The histocompatibility antigen HLA-B27, which does not exist in Black Africans of unmixed ancestry, is present in 8 percent of White and only about 2-4 percent of the Black American population (reflecting racial mixing).
Susceptibility to the coronavirus is negatively associated with having a genetic propensity to absorb Vitamin C, as is the case with Black African populations. Across Africa, roughly 50 percent of people carry the Vitamin C-friendly variant and in some African countries, it is as high as 70 percent. In the US, 41 percent of Whites carry this variant, compared to 55 percent of Blacks, and only 31 percent of Asians.
There is also preliminary evidence to suggest that vitamin D supplements at high doses might help protect against becoming infected with COVID-19 or limiting serious symptoms. How might this relate to people of African ancestry? Blacks as a population group have markedly low levels of vitamin D.

Yet in a paradox, people of African ancestry who take Vitamin D supplements get no skeletal benefits from taking supplements. Their bones are naturally less brittle than those of other populations. Black Americans, for example, have significantly fewer incidences of falls, fractures or osteopenia compared to White Americans.
Could the factors that naturally protect the bone health of Blacks also protect them against more serious COVID symptoms? At the moment, there are no clear explanations for the vitamin D ‘Black paradox,’ but scientists we talked to say there may be some genetic factors at play.
Genetics cuts multiple ways – it can protect or increase vulnerabilities, or do both at the same time
Are Black Americans and those of African descent in general less genetically susceptible to some viruses or diseases other than COVID-19? The evidence is fragmentary. Contradicting racist early 20th century theories that ‘frail’ Blacks are more susceptible to disease, during the 1918 pandemic the incidence of influenza was significantly lower in African Americans.
And according to one 2016 study of swine flus, when exposed to flu, “African Americans mounted higher virus neutralizing and IgG antibody responses to the H1N1 component of IIV3 or 4 compared to Caucasians”.
The relationship of genes to disease is often convoluted. Populations of African descent simultaneously are more prone to sickle cell anaemia (particularly prevalent south of the Sahara) and have natural, genetic-based defenses against malaria. This connection was noted over 50 years ago.
And In a tragic twist, some genetic variants thought to reduce susceptibility to malaria are believed to increase vulnerability to the HIV virus. While fear of AIDS has receded in the West and in developing countries in Africa, HIV still infects tens of millions of people, with hundreds of thousands dying of the disease each year, mostly in Africa. Adult HIV prevalence is 1.2 percent worldwide but 9 percent in sub-Saharan Africa.
In the US, where the national rate is 0.6 percent, African Americans, account for 42 percent of new HIV infections despite being only 12 percent of the population. It’s now believed that a gene variant common in some African and African diaspora populations that protects against certain types of malaria increases susceptibility to HIV infection by 40 percent.
If this is indeed the case, it is an example of genes conferring both benefits and liabilities as populations evolved and moved around in different eras in different environments. In ancestral environments, malaria was the force selecting for variants that provided partial immunity; in the modern environment, HIV may be the force selecting against those unfortunate enough to carry these genetics might partly explain the apparent reduced severity of COVID-19 in Africa.
Patrick Whittle has a PhD in philosophy and is a New Zealand-based freelance writer with a particular interest in the social and political implications of biological science. Follow him on his website patrickmichaelwhittle.com or on Twitter @WhittlePM
Jon Entine is the founding editor of the Genetic Literacy Project, and winner of 19 major journalism awards. He has written extensively in the popular and academic press on population genetics, including two best-sellers, Taboo: Why Black Athletes Dominate Sports and Why We’re Afraid to Talk About It; and Abraham’s Children: Race, Genetics and the DNA of The Chosen People. Follow him on Twitter @JonEntine
Image par FrankundFrei de Pixabay