A study published on 19 December in Nature Communications has shown that the active ingredient in eyedrops originally being developed to treat eye disease may be effective in treating an aggressive form of leukaemia (1).
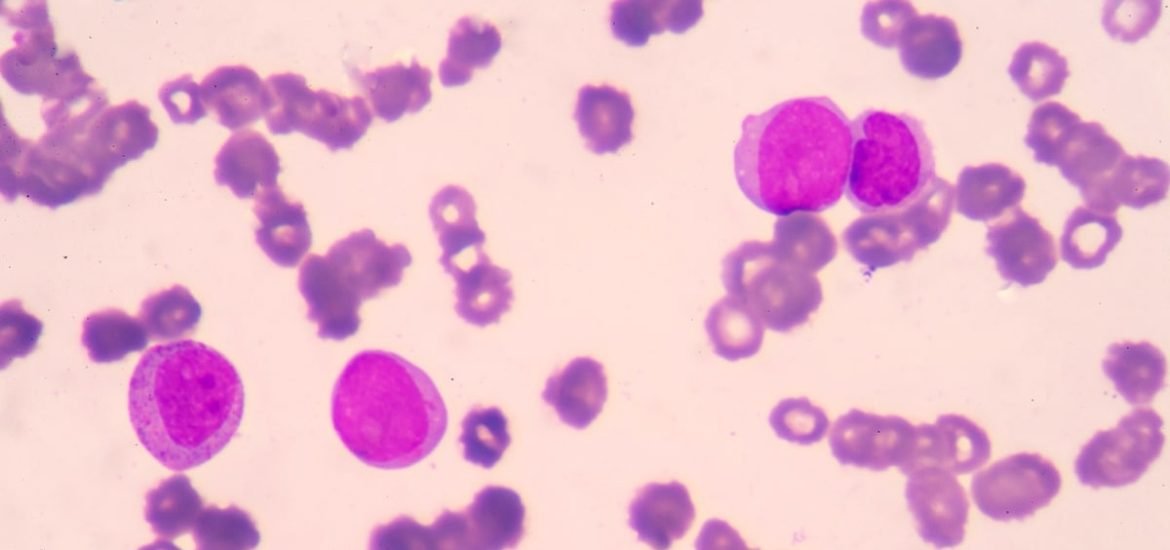
Acute myeloid leukaemia (AML) is a type of blood cancer that begins in the myeloid cells ― precursor cells that form red blood cells, platelets, and some white blood cells ― found in bone marrow. The term “acute” is given to the condition since it progresses rapidly, which can affect people of all ages. While there is currently no known cure, treatments like chemotherapy can lead to remission, however, months of intensive chemotherapy and prolonged hospital stays are often required.
Scientists from the Wellcome Sanger Institute, University of Cambridge, University of Nottingham, and other collaborators discovered a certain compound targets a particular cancer gene and could, therefore, destroy the leukaemia cells without harming healthy blood cells.
Previous attempts by researchers from the Sanger Institute to develop approaches using the CRISPR-Cas 9 gene editing technology were able to identify more than 400 genes as possible therapeutic targets (2). In particular, the SRPK1 gene ― involved RNA splicing, part of the process used by cells to produce proteins ― is critical to the growth of a certain subset of cancer cells, MLL-rearranged AML.
The current findings show that genetic disruption of SRPK1 halts the growth of MLL-rearranged AML cells. Moreover, the SPHINX31 compound ― a compound found in an eye drop treatment currently being developed for retinal neovascular disease ― strongly inhibits the growth of several MLL-rearranged AML cell lines, but interestingly, not the growth of normal blood stem cells. The scientists used something called “rescue experiments” to ensure the observed effect were due to knockdown of the target gene and not other factors. When patient-derived human AML cells were implanted mice treated with the compound, AML cell growth was strongly inhibited, thus showing promise as a potential approach for treating the aggressive form of leukaemia in human.
The SRPK1 inhibition causes changes to another well-known gene, BRD4, which is known to play a role in leukaemia cell maintenance. The authors write, “the BRD4 isoform switch is one key mediator of the anti-leukemic effects of this compound. In other words, changes in BRD4 lead to “anti-AML effects.” Furthermore, they suggest the approach could potentially be used to treat other cancers, such as metastatic breast cancer, in which BRD4 plays a crucial role.
Importantly, the study has described a novel mechanism required for leukaemia cell survival and highlights the therapeutic potential of SRPK1 inhibition. By inhibiting this key gene using a novel compound found in eye drops, the growth of an aggressive form of acute myeloid leukaemia can be stopped. New treatments will, of course, take some time to reach the clinic, however, the results highlight the potential of “modulation of splicing” as a promising therapeutic approach in leukaemias.
(1) Tzelepis, K. et al. SRPK1 maintains acute myeloid leukemia through effects on isoform usage of epigenetic regulators including BRD4. Nature Communications (2018) DOI: 10.1038/s41467-018-07620-0
(2) Tzelepis, K. et al. A CRISPR dropout screen identifies genetic vulnerabilities and therapeutic targets in acute myeloid leukemia. Cell Reports (2016). DOI: 10.1016/j.celrep.2016.09.079