A new study published on 13 February in Nature has demonstrated that persistent disruption to sleep increases white blood cell production causing damage to blood vessels (1). The researchers showed that when sleep is disturbed, the brain signals to the bone marrow to increase the production of white blood cells which triggers an inflammatory response in mice.
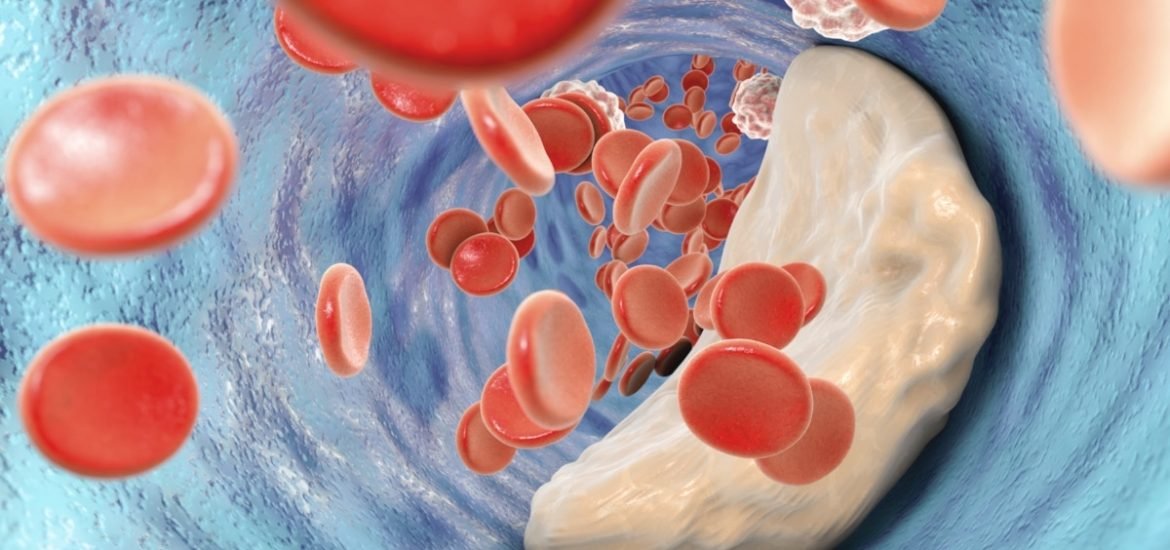
Poor or insufficient sleep is a major public health problem affecting millions of people worldwide. Disturbed sleep or “sleep fragmentation” has long been associated with an increased risk of cardiovascular diseases, such as atherosclerosis ― a buildup of plaque within artery walls which restricts blood flow (2). However, the cellular and molecular mechanisms of these effects remain poorly understood.
An international team of researchers have now discovered that mice with disturbed sleep exhibit more severe atherosclerosis ― accompanied by an increase in white blood cells in the bone marrow and in the blood ― whereas mice kept fully awake did not experience the same effects. Furthermore, a previously unknown mechanism between the brain, bone marrow, and blood vessels seems to protect against the development of atherosclerosis.
The researchers genetically engineered mice to develop atherosclerosis and then disrupted their sleep patterns. Mice with disrupted sleep developed larger arterial plaques or fatty deposits ― up to one-third larger ― compared to control mice. In addition, sleep-disrupted mice produced twice the level of certain inflammatory cells in their blood.
Interestingly, the scientists did not find any connection between sleep deprivation and the ‘fight-or-flight’ response activated by the sympathetic nervous system, which is known to increase the production of white blood cells and atherosclerosis. Instead, they found reduced production of an important neuropeptide called hypocretin ― regulates arousal, wakefulness, and appetite ― in sleep-deprived mice. Moreover, similar to sleep-deprived mice, those that that had been genetically modified to be unable to express hypocretin also produced more white blood cells and had increased atherosclerosis.
But when sleep-deficient, atherosclerotic mice were administered hypocretin supplements, the scientists observed fewer inflammatory cells and the mice developed smaller atherosclerotic plaques. In addition, the authors found that reduced hypocretin led to an increase in another protein called colony-stimulating factor 1 (CSF-1), which also increases the production of white blood cells, and in particular, monocytes, which promotes atherosclerosis.
However, other mechanisms besides the hypocretin–CSF-1 pathway may also be involved, as the authors acknowledge. Therefore, more studies are needed to fully uncover the links between sleep disorders and cardiovascular conditions, and could potentially lead to new treatments.
Nonetheless, the study highlights the importance of getting enough quality sleep to maintain cardiovascular health. The anti-inflammatory pathway regulated by sleep breaks down when sleep is disrupted and may help explain some of the links between sleep and cardiovascular health, as well as an increased risk of obesity, diabetes, and cancer.
(1) McAlpine, C.S. et al. Sleep modulates haematopoiesis and protects against atherosclerosis. Nature (2019). DOI: 10.1038/s41586-019-0948-2
(2) Cappuccio, F.P. et al. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European Heart Journal (2011). DOI: 10.1093/eurheartj/ehr007