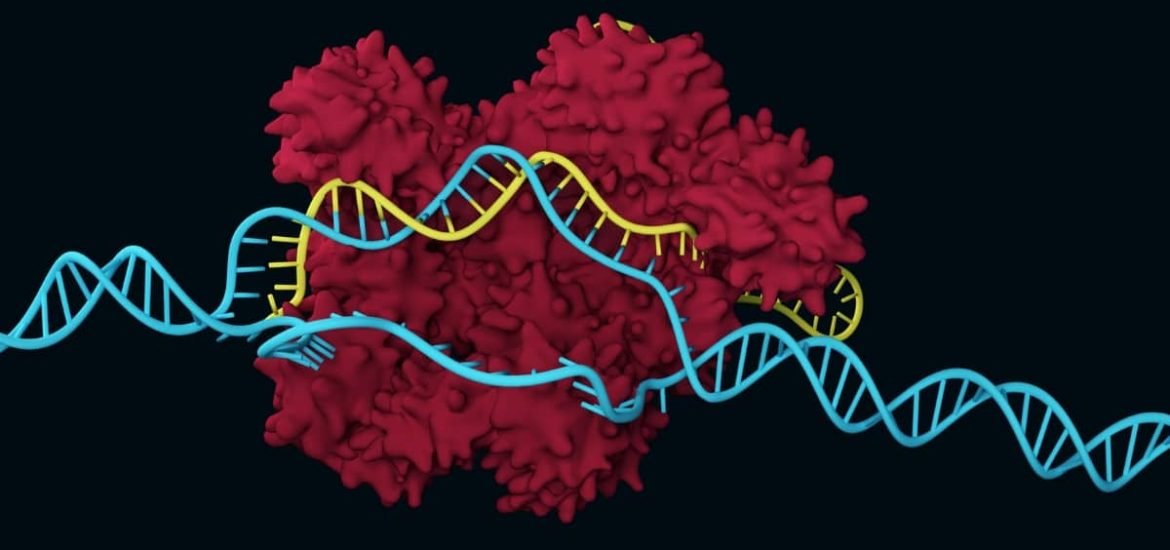
Two separate studies published on 8 October in Nature Medicine have successfully used modified CRISPR-Cas9 gene editing technologies to correct gene mutations associated two genetically inherited metabolic disorders, phenylketonuria and hereditary tyrosinemia type 1 (HT1). The use of base editors in the modified gene-editing systems essentially sidesteps the need to cut DNA ― a drawback of traditional CRISPR/Cas editing that can lead to unintended genetic errors ― and instead, an enzyme is used to modify the genetic sequences and produce therapeutic effects.
The team of researchers, led by Gerald Schwank from ETH Zurich, took advantage of the modified CRISPR-Cas9 gene editing technology to correct mutated genes in the liver cells of mice with phenylketonuria. They paired the CRISPR-Cas9 system with an enzyme called cytidine deaminase ― which converts the DNA base pair mutation into a healthy base pair ― and packaged them into an adeno-associated viral vector which was injected it into the blood of adult mice (1). The authors reported that up to 60 per cent of the copies of the mutated genes were corrected, phenylalanine levels returned to normal, and the symptoms of phenylketonuria were reversed.
Phenylketonuria, a rare liver disease, is caused by defective genes for phenylalanine hydroxylase and a lack of functional phenylalanine hydroxylase causes a toxic buildup of phenylalanine. Without the phenylalanine hydroxylase enzyme, phenylalanine cannot be metabolized resulting in a variety of symptoms, including atopic dermatitis, seizures, and cognitive delays. According to first author Lukas Villiger, a doctoral candidate, “The use of a base editor was the key to our success.”
In another study, scientists paired CRISPR-Cas9 with base editor 3, which converts one DNA base into another, to treat a rare liver disease, HT1 (2). This time, instead of targeting the disease-causing gene mutation, the gene editing tool was used to disable a different gene, HP1, in prenatal mice. The scientists gently opened the uterus of a pregnant mouse, removed the fetus from the amniotic sac, and injected the CRISPR-loaded adenovirus vector into the vitelline vein of the fetus, which is connected to the liver. The fetus was then placed back in the uterus and born as normal.
Similar to phenylketonuria, the disease can be managed by adhering to a strict diet and also by taking a drug called nitisinone but can develop into liver failure or cancer. After birth, gene-edited mice survived longer and gained more weight compared to control mice that had received the usual phenylketonuria treatments. In addition, the authors reported that mice carried stable amounts of BE3-edited liver cells for three months. Kiran Musunuru from the Perelman School of Medicine told STAT, “We weren’t expecting it, but the genome-edited mice did much better.” In another statement on the research, Musunuru said, “We also plan to use the same base-editing technique not just to disrupt a mutation’s effects, but to directly correct the mutation.”
Traditional gene therapy transfers an entire healthy gene, typically by a virus, into cells to replace the disease-causing gene, whereas CRISPR only alters the mutated portion of a defective gene and therefore, may provide a safer, more effective approach. Both proof-of-principle studies offer hope that gene editing could be effectively used in the future to correct genetic defects. Moreover, fetal gene editing could stop disease progression before it causes irreversible or fatal damage.
(1) Villiger, L. et al. Treatment of a metabolic liver disease by in vivo genome base editing in adult mice. Nature Medicine (2018). DOI: 10.1038/s41591-018-0209-1
(2) Rossidis, A.C. et al. In utero CRISPR-mediated therapeutic editing of metabolic genes. Nature Medicine (2018). DOI: 10.1038/s41591-018-0184-6
Amazing, hope we’ll see treatments for genetic diseases for humans too soon