This year, the Nobel Prize in Physiology or Medicine was awarded to three biologists who helped decipher how cells of the body sense and adapt to available oxygen. These advances have been crucial to our current understanding — and ultimately, treatment — of disease.
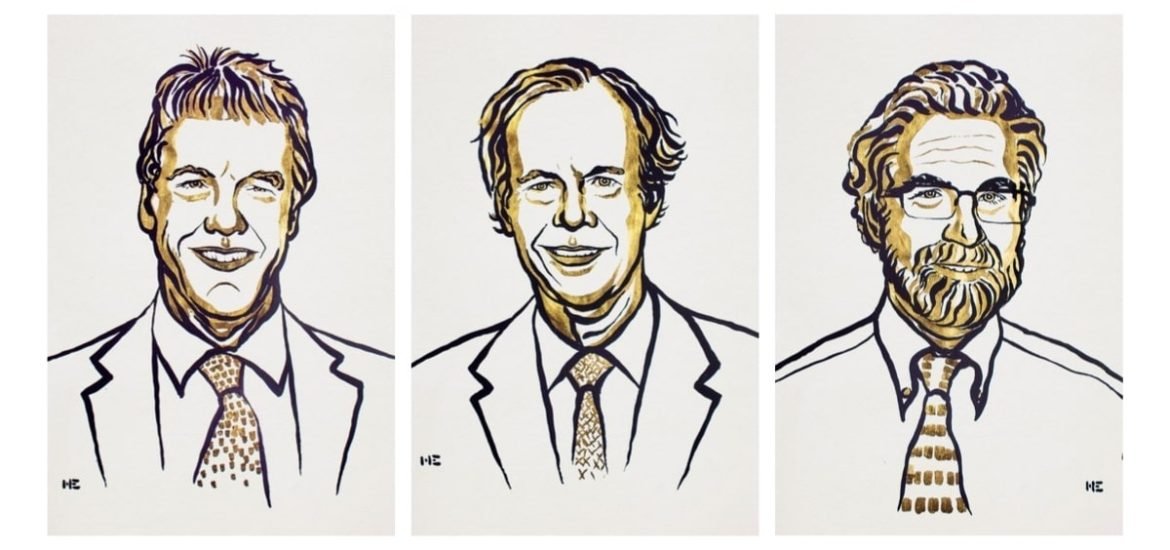
The prize was jointly awarded to Prof William Kaelin, Jr. of the Dana-Farber Cancer Institute in Boston, Massachusetts, Sir Peter Ratcliffe, physician-scientist affiliated with the University of Oxford and the Francis Crick Institute in London and Prof Gregg Semenza at the Johns Hopkins University School of Medicine. The same researchers were also awarded the prestigious Albert Lasker Basic Medical Research Award in 2016.
The work, which has spanned more than 20 years, has led to the development of various drugs to treat anaemia, heart disease, and lung cancer. In addition, this knowledge is being used to develop novel strategies for combatting cancer.
Why is oxygen so important?
How the body responds to oxygen levels is one of the most fundamental processes for life. When cells sense low oxygen levels (referred to as hypoxia), they respond by creating new blood cells and blood vessels. This crucial physiological process explains how some animals, including humans, can adapt to living at high-altitudes where the levels of oxygen in the outside air are much lower.
The oxygen we breathe in is used by cells to convert food into useful energy in a process called cellular respiration. Cells then use this energy to perform vital functions. However, if there is not enough oxygen available, the scientists discovered that a protein called hypoxia-inducible factor, or HIF, builds up in cells, and can have a number of different effects.
Semenza and Ratcliffe showed that HIF triggers the production of an important hormone called erythropoietin (EPO), which in turn, boosts the number of oxygen-carrying red blood cells. In this way, our bodies have the incredible ability to adapt to different oxygen levels, for example, during intense exercise. And even the immune system can be tweaked according to the body’s oxygen-sensing mechanism. Without this essential protein, cells would not survive past the early development stages in the embryo. And patients with chronic renal failure often suffer from severe anaemia as a result of decreased EPO expression.
The work of Kaelin’s group showed that another gene called VHL is also involved in how cells respond to oxygen. A mutation in the VHL can increase the risk of certain cancer. Later, Ratcliffe and his team revealed interactions between VHL and HIF that may actually lead to the destruction of HIF in low-oxygen conditions.
In 2001, Kaelin and Ratcliffe both demonstrated that chemical modification of the VHL protein allows cells to rapidly respond to oxygen levels. This led scientists to investigate promising drugs, such as prolyl hydroxylase inhibitors, for treating anaemia and renal failure by preventing VHL from binding to HIF and causing its degradation.
Oxygen-sensing processes also play an important role in cancer. Oxygen regulation by cancer cells can stimulate the growth of blood vessels inside tumours allowing them to effectively grow. And based on this essential discovery, scientists are now pursuing novel cancer treatments that rely on blocking interactions between oxygen-sensing machinery of the body and cancer cells.
Photo credit: Ill. Niklas Elmedhed/ Nobel Media.